Samuel Shem Calls for Using VistA and the VA Model of Care to Solve the Physician Burnout Crisis
 Roger A. MaduroOn November 1st Newsweek published an extraordinary Op-Ed by Samuel Shem titled Why Computerized Medical Records Are Bad for Both You and Your Doctor. In the article, Shem, pen name for the American psychiatrist and well-known author Stephen Joseph Bergman, presents evidence that poorly designed electronic medical records (EMRs) and over-regulation are to blame for the growing crisis of physician burnout and suicide. The rate of suicides among physicians has risen to a staggering number--three per day. Shem argues that there is a "better way," and that is shown by the electronic health record (EHR) system used by the U.S. Department of Veterans Affairs (VA). The VA's EHR is called VistA. Shem's view is supported by a large and increasing number of physicians and nurses. And solving the physician burnout crisis is becoming a major issue in the current presidential elections. It will be an issue that has to be addressed by all candidates.
Roger A. MaduroOn November 1st Newsweek published an extraordinary Op-Ed by Samuel Shem titled Why Computerized Medical Records Are Bad for Both You and Your Doctor. In the article, Shem, pen name for the American psychiatrist and well-known author Stephen Joseph Bergman, presents evidence that poorly designed electronic medical records (EMRs) and over-regulation are to blame for the growing crisis of physician burnout and suicide. The rate of suicides among physicians has risen to a staggering number--three per day. Shem argues that there is a "better way," and that is shown by the electronic health record (EHR) system used by the U.S. Department of Veterans Affairs (VA). The VA's EHR is called VistA. Shem's view is supported by a large and increasing number of physicians and nurses. And solving the physician burnout crisis is becoming a major issue in the current presidential elections. It will be an issue that has to be addressed by all candidates.
The growing movement for VistA poses an interesting paradox. In May 2018 the VA announced they had decided to replace VistA with the commercial Cerner system. Since the VA has been the primary developer of VistA, how can hospitals in the private sector replace their poorly designed and very expensive medical billing EMRs with VistA? We will discuss the paradox and potential solutions in this article.
But first, let's hear what Shem had to say in his Newsweek article.
"A Better Way?"
In the first part of the article, Shem argues that the fundamental problem with EMRs is that they have been turned into "cash registers." Their primary purpose has become "to bill the most for your treatment." As a result, the core clinical component function of EMRs "became coding diagnoses and treatments for payment."
Shem posits that there is a better way. He states:
"Recently, I was speaking with medical students about their training on the wards. They are discouraged about the lack of instruction from the residents. Patient rounds are now conducted using portable screens rolling up and down the corridor. The team rarely enters a patient's room. Rounds over, the residents break for their computers, trying to get in all their clicks. The students are stranded. They are screen-savvy millennials, yet they call Epic a terrible system. I ask if they know of a better one.
"Yes," said one, "the Veterans Administration." I asked why. "Well, their system is kind of clunky, but you can input notes about your patients, it's easy to understand, and it links to VAs all over the world. " I ask about the differences between Epic and the VA. They consider. "There's no billing at the VA," one says. "It's not for profit." Others agree. In the EMR machine, patient care is linked tightly to billing. To improve patient care, we have to unlink them, and squeeze out the for-profit billing.
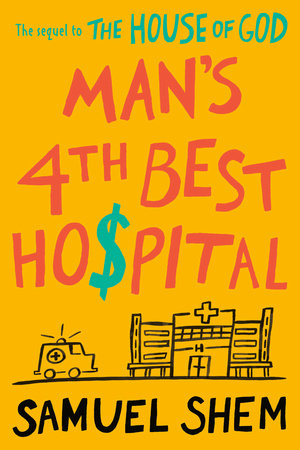
 Samuel ShemShem then proposes VistA and the VA model of care as a solution to the healthcare crisis in the U.S. And this is just an article. Shem has written an entire book that examines the impact of the takeover of medicine by "the machines." He presents an alternative approach. Titled Man's 4th Best Hospital this book was just released by Penguin Random House. The book has already received rave reviews from leading healthcare industry experts. It is a sequel to Shem's bestselling and highly acclaimed book The House of God. If the original book's success is a metric to go by, Shem's book should be a huge hit. The House of God became a must-read book by physicians and sold over a million copies.
Samuel ShemShem then proposes VistA and the VA model of care as a solution to the healthcare crisis in the U.S. And this is just an article. Shem has written an entire book that examines the impact of the takeover of medicine by "the machines." He presents an alternative approach. Titled Man's 4th Best Hospital this book was just released by Penguin Random House. The book has already received rave reviews from leading healthcare industry experts. It is a sequel to Shem's bestselling and highly acclaimed book The House of God. If the original book's success is a metric to go by, Shem's book should be a huge hit. The House of God became a must-read book by physicians and sold over a million copies.
On the Future of VistA
The big question, however, is whether VistA has a long-term future. As mentioned, the VA has decided to phase out VistA and replace it with Cerner's medical billing EMR. Up until recently, the VA has been the primary developer of VistA. That said, the Cerner deployment is going to take more than a decade. Therefore, the VA is going to continue supporting the development of VistA for the next decade and potentially longer than that.
The next question then is whether VistA development could continue as the VA winds down their contributions. This is the part of the story where we shift from the VA being the principal user of VistA to the new paradigm where there are more implementations and instances of VistA outside the VA medical system than in the VA.
VistA is thriving outside the VA and is already being rapidly modernized. The challenge is not the continuing improvement and modernization of VistA, it is to gather the efforts of the community together to accelerate those developments. The VistA community is highly fragmented and is going in too many directions. What is needed is an open source Universal Health Record (UHR) as outlined in an article by Dr. Bruce Wilder (see here).
This concept was the foundation of H.R. 6898 introduced by Congressman Pete Stark (D-CA) on September 15, 2008. The bill called for the establishment of a federal open source Health IT system. The idea was to develop an open source EHR that could be used by Federal, State, local, and tribal agencies and medical facilities, as well as the private sector. Commercial EMR vendors were opposed to an open source EHR, so they spent over $100 million lobbying campaign against the Stark Bill and defeated it. They then wrote what became the HITECH Act of 2009 which is the foundation of the present broken medical records system and what has led to the physician burnout crisis.
 It is now up to the private sector to modernize VistA. It is for this reason that Joel Mewton, a leading member of the VistA community and Chief Technical Officer of Bitscopic, proposed Project Hilleman. The purpose of the project is to bring VistA adopters together in an open source way to work on VistA modernization. OSEHRA featured Project Hilleman in one of their popular Innovation Webinars. A recording of Mewton's presentation is available here.
It is now up to the private sector to modernize VistA. It is for this reason that Joel Mewton, a leading member of the VistA community and Chief Technical Officer of Bitscopic, proposed Project Hilleman. The purpose of the project is to bring VistA adopters together in an open source way to work on VistA modernization. OSEHRA featured Project Hilleman in one of their popular Innovation Webinars. A recording of Mewton's presentation is available here.
That is a topic unto itself that merits a whole article that we hope to publish in the future. The immediate question posed by Shem's article and book is whether hospitals and medical facilities can successfully migrate from their medical billing EMRs to VistA? The answer is a resounding YES!
Some key factors regarding the status of VistA.
- Year after year VistA is ranked as the top EHR in the world in terms of user satisfaction and usability. No surprise here as VistA was designed by physicians for physicians. During the "Golden Age" between 5,000 to 10,000 phsycians, nurses, clinicians, and other staff were involved in supporting the development of VistA.
- VistA is still considered the world's best hospital-based EHR.
- VistA is open source software which means that it can be adapted and modified by the users. And it has a large community adding code to the EHR.
- VistA implementation, support, and maintenance costs are only a fraction of the cost of medical billing EMRs.
- More than 100 VistA implementation in the private sector and state hospitals in the U.S. show that implementations cost just 5% to 30% of the implementation costs of comparable medical billing EMRs.
- Running cost differentials are even starker at hospitals running VistA. The operating costs of VistA are, in general, less than 5% of the operating costs of medical billing EMRs. VistA is easy to support, configure, enhance and maintain and has no recurring licensing fees.
Here is some background information regarding VistA adoption:
- VistA is thriving outside the VA. Estimates are that there are more than 2,500 medical facilities around the world running VistA. The VA has a total of 1,255 medical facilities.
- The number of medical facilities implementing VistA, particularly those in foregin countries, is growing rapidly.
- There are more than 100 hospitals in the U.S. outside of the VA running VistA or VistA derivatives such as the Indian Health Service's RPMS.
- There are more than 1,000 clinics and physician offices in the U.S. running VistA or a VistA-derivative outside of the VA medical system.
- Other nations and large medical systems around the world consider that VistA is the best hospital-based EHR in the world. There is a bright future for VistA in other countries where its EHRs capabilities are better appreciated. This is particularly the case in the Kingdom of Jordan and in India. Many other countries have a growing base of VistA installations.
- More than 30 major hospitals in India, most with more than 1,000 beds, have implemented VistA. There is even a hospital with more than 10,000 beds running VistA. In addition, VistA has been implemented in many clinics and adjacent facilities.
- The Kingdom of Jordan has self-implemented VistA throughout the country. More than 85% of all medical facilities in Jordan are now running on Jordan's own, advanced and modernized version of VistA. A nation of more than 10 million people (plus more than two million refugees), Jordan does not have many natural resources. It is leveraging their human capital, which includes highly educated and capable medical professionals, to become the primary destination from people in the Middle East and Africa seeking high-quality medical care. VistA plays a major role in increasing the quality of medical care they provide.
- More recently, the team that implemented, configured, and enhanced VistA in Jordan, is now deploying VistA in other countries in the Middle East.
Can you give us some examples?
Many argue that in the U.S. VistA can only function in single-payer systems. Below are two of over a hundred examples that demonstrate the contrary. One is from a private-sector regional hospital in Northern California, and the other is a State hospital in North Carolina.
 Robert WentzOroville Hospital, a 133-bed regional hospital in Northern California, is a great example of how VistA can be successfully implemented in the private sector at a fraction of the cost of commercial systems. Oroville Hospital has been consistently ranked among the top US hospitals in terms of quality measures. They accomplished their VistA implementation and quality of care at a fraction of the cost of what other hospitals have spent in their medical billing EMR systems.
Robert WentzOroville Hospital, a 133-bed regional hospital in Northern California, is a great example of how VistA can be successfully implemented in the private sector at a fraction of the cost of commercial systems. Oroville Hospital has been consistently ranked among the top US hospitals in terms of quality measures. They accomplished their VistA implementation and quality of care at a fraction of the cost of what other hospitals have spent in their medical billing EMR systems.
As detailed in this blog post, Robert Wentz, CEO of Oroville Hospital gave a detailed presentation at the VistA EXPO 2011 conference in Seattle, describing all the steps that led to the decision to implement VistA. According to Wentz, "the Oroville staff met with virtually every single commercial EHR vendor in the country. The decision to go with VistA was taken only after reviewing all other options." According to Wentz, the numbers were clear, implementing a commercial EHR would have put the regional hospital out of business.
Oroville's decision to self-implement VistA was recently examined in depth by the most demanding researchers. Last year the hospital went to the capital markets seeking $200 million in bonds to build a new 5-story hospital building and expand their personnel and services. The bond offering was managed by the Morgan Stanley investment bank.
Quotes from this article from the February 14, 2019, Sacramento Bee provides the details of the bond sale.
According to Wentz, "he wasn't certain how the offering would go but decided to let employees watch the sale on a monitor in a lounge at the hospital. It turned out there was far more demand than supply for the bonds, however. 'In 24 minutes, the $200 million just gets snapped up,' Wentz said. 'We thought maybe we would get two times the amount of orders than what's offered...We see the orders going up to $350 million, then $500 million, then $700 million, then $800 million. We didn't think that was possible, but it continued, and the orders that came in were $1.035 billion.'
The Sacramento Bee continues.
"I called one of our advisers to ask: 'How normal is this?'" Wentz said. "He'd been in this business for 37 years, and he told me, 'I'm taking a picture of my computer screen right now.'...I was also excited that this market, this big huge financial market we have in this country still feels like an independent hospital in California is still a good investment."
In other words, the leading investment firms in the United States, after thorough research, placed a billion-dollar bet on VistA for a rural, regional hospital. All these investment firms have detailed financial data on all hospitals in the United States. Hundreds of hospitals across the U.S. have been driven into bankruptcy and closure due to the high cost of commercial EMRs, and hundreds more are in danger of closing down by the end of next year. Rural and critical access hospitals are in serious trouble across the U.S.
What makes Oroville Hospital the exception? To say VistA is a clear and simple answer. But there are many additional stories to tell in the future, as it involves an enormous amount of work and dedication on the part of the Oroville Hospital staff and leading VistA developers to modernize and improve Oroville's VistA (OroVistA), and to leverage it to improve patient care as well as to streamline hospital operations while reducing costs and expenditures. There are literally more than 120 posts in Open Health News related to the Oroville Hospital story.
 Oroville Hospital went to the bond markets to raise $200 million to build this expansion wing for the hospital. They got bids totaling over one billion dollars.Robert Wentz and the Oroville Hospital team are committed to sharing all the improvements they are making to Vista with others. They have licensed all the code under the Apache Software license. They believe that if other hospitals were to implement VistA, then they could all share and help each other. That is the core of the Universal Health Record concept.
Oroville Hospital went to the bond markets to raise $200 million to build this expansion wing for the hospital. They got bids totaling over one billion dollars.Robert Wentz and the Oroville Hospital team are committed to sharing all the improvements they are making to Vista with others. They have licensed all the code under the Apache Software license. They believe that if other hospitals were to implement VistA, then they could all share and help each other. That is the core of the Universal Health Record concept.
Oroville Hospital is not the only example. Another one is North Carolina's Central Regional Hospital (CRH), a state psychiatric and medical facility located in Butner, North Carolina. The 398-bed hospital serves the acute and long-term inpatient mental health and medical needs of North Carolina citizens from 26 counties and employs more than 1,900 staff, including 50 doctors, 300 professional nurses, 700 nursing assistants, 40 psychologists, and 70 social workers. Central Regional Hospital is a major teaching site for 23 psychiatric residents per year from Duke University and the University of North Carolina medical schools. It also provides training for medical students from both schools as well as psychiatry subspecialty fellowship training.
After years of research, the hospital staff decided to self-implement VistA. The State had no funds to implement EHRs in the State medical facilities. By implementing the open source VistA, CRH was able to implement a full EHR that they could customize themselves to their needs by just using labor. CRH did not have to pay licensing fees so they used their existing personnel budget to hire VistA experts and implemented VistA with support and advice from Oroville Hospital and the VistA community they self-implemented VistA. The VistA implementation was, and continues to be, a complete success, and came in at less than one million dollars. Full details of the CRH implementation can be found in this article.
As noted above, CRH is just down the road from Duke University which sends many of their medical students to do their residency programs at CRH. In sharp contrast to CRH, Duke University Hospital went with a commercial EMR, Epic Systems. So far Duke University has spent over a billion dollars in its EMR implementation!
Conclusion
Samuel Shem's book, Man's 4th Best Hospital is clearly going to trigger a long-needed examination and debate on the role of "the machines" in the practice of medicine, as well as the changes needed to fix America's broken healthcare system. Interestingly enough, the caption in one of the photos in the Op Ed points to the success of EHRs in improving medical care in "Third World" countries. The caption reads "An Ivorian doctor uses a tablet computer in Bouake hospital's as part of a telemedicine project, but in the U.S. having computerized medical records is putting a greater emphasis on billing rather than care, argues Samuel Shem..." Shem is correct in that while VistA is superior to the medical billing EMRs, it does need to be modernized. VistA deployments in the U.S. and other countries show that VistA can be modernized, and the VA model of care can be a success.
- Tags:
- American Journal of Medicine
- Andrew Alexander
- Bitscopic
- Bruce Wilder
- clinical data
- Computerized Medical Records
- doctor burnout epidemic
- Duke University Hospital
- Electronic Medical Record (EMR)
- EMR machine
- Epic
- for-profit billing
- Harvard Business School
- HR6898
- Joel Mewton
- Journal of the American Medical Association (JAMA)
- Kaiser Health News
- Kenneth Ballou
- Maslach Burnout
- Medicaid
- Medicare
- national health care system
- national public health care system
- North Carolina Central Regional Hospital
- Oroville Hospital
- patient medical history
- physician moral injury
- physicians burni out epidemic
- Project Hilleman
- Robert Wentz
- Samuel Shem
- Simon G. Dean
- Stark bill
- universal health record
- US Department of Veterans Affairs (VA)
- Veterans Administration
- Veterans Health Administration (VHA)
- VistA EHR
- Wendy Dean Talbot
- The Future Is Open
- Login to post comments