The delivery of public health information systems relies on the concerted convergence of people, process, and technology in a disciplined manner. This is not to say that one is more important than the other, but that they must be applied consistently over the system development life cycle to ensure a quality product. Gone are the days of simply letting your Information Technology staff know what you were looking for or what you thought you wanted. Today, the need to fully comprehend and articulate the problem you are hoping to solve will not only clarify the need but present the case for change to obtain agreement of key partners, including your own staff. I often hear we thought everyone was on board with our desire to migrate to a new system, only to find out our own staff did not understand our desire to move off a system that everyone was familiar and comfortable with using. Our own staff?!
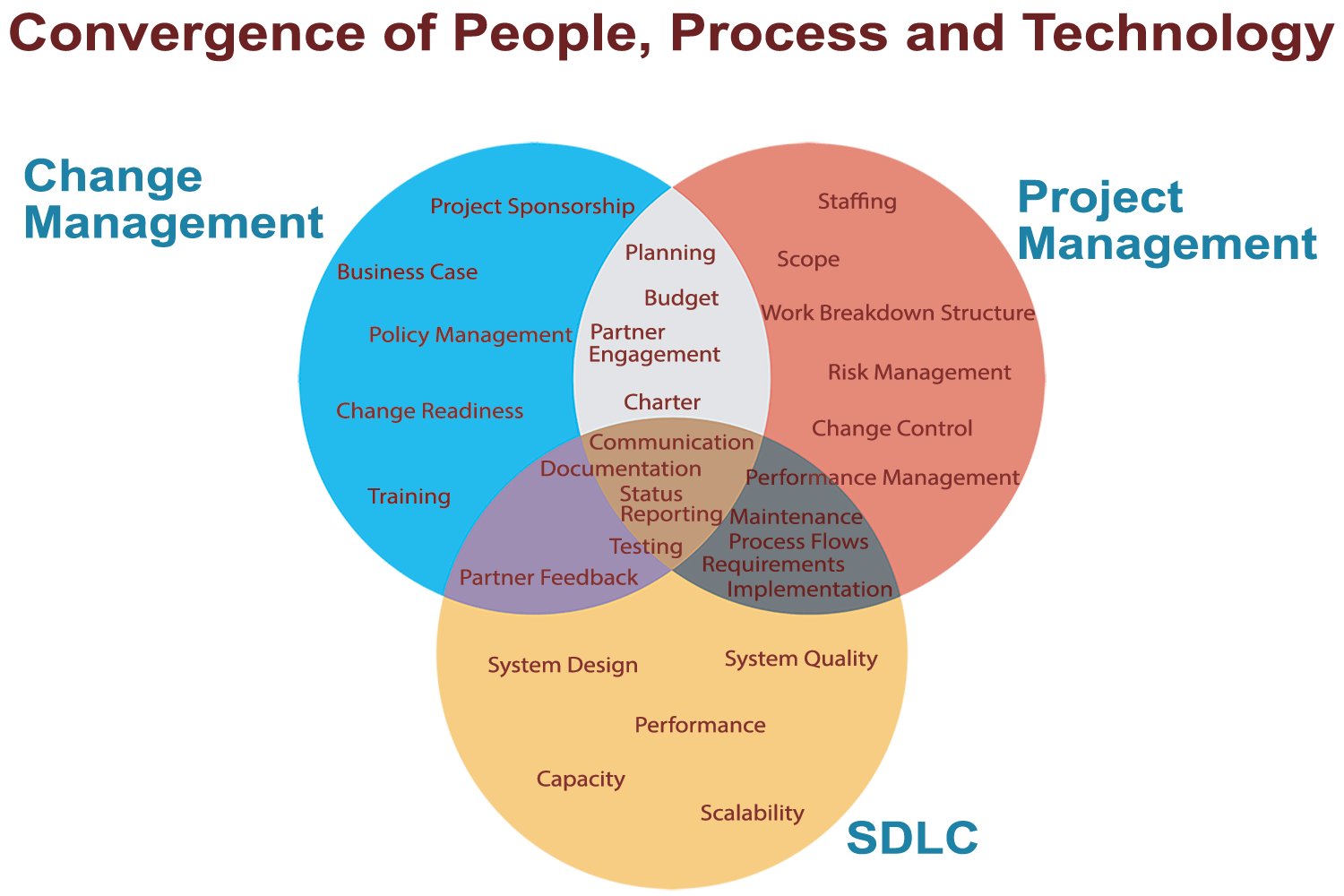
This is precisely the reason to apply change management principles to raise internal staff and external partners’ awareness of the need for change and effectively communicate throughout the project to keep them apprised of the progress being made and the actions being taken to effect change. Other change management efforts to assist staff and partners through a transition include engaging them in various activities, such as requirements collection and process re-engineering, as well as providing training to make them more knowledgeable of and familiar with the new system.
Just as integral as change management, project management discipline focuses on the project scope, resources and timeline to ensure a smooth transition. With an eye toward process and planning, project management allows for consistent engagement of project partners through status reporting and testing for validation that the requirements and process flows yield their expected results.
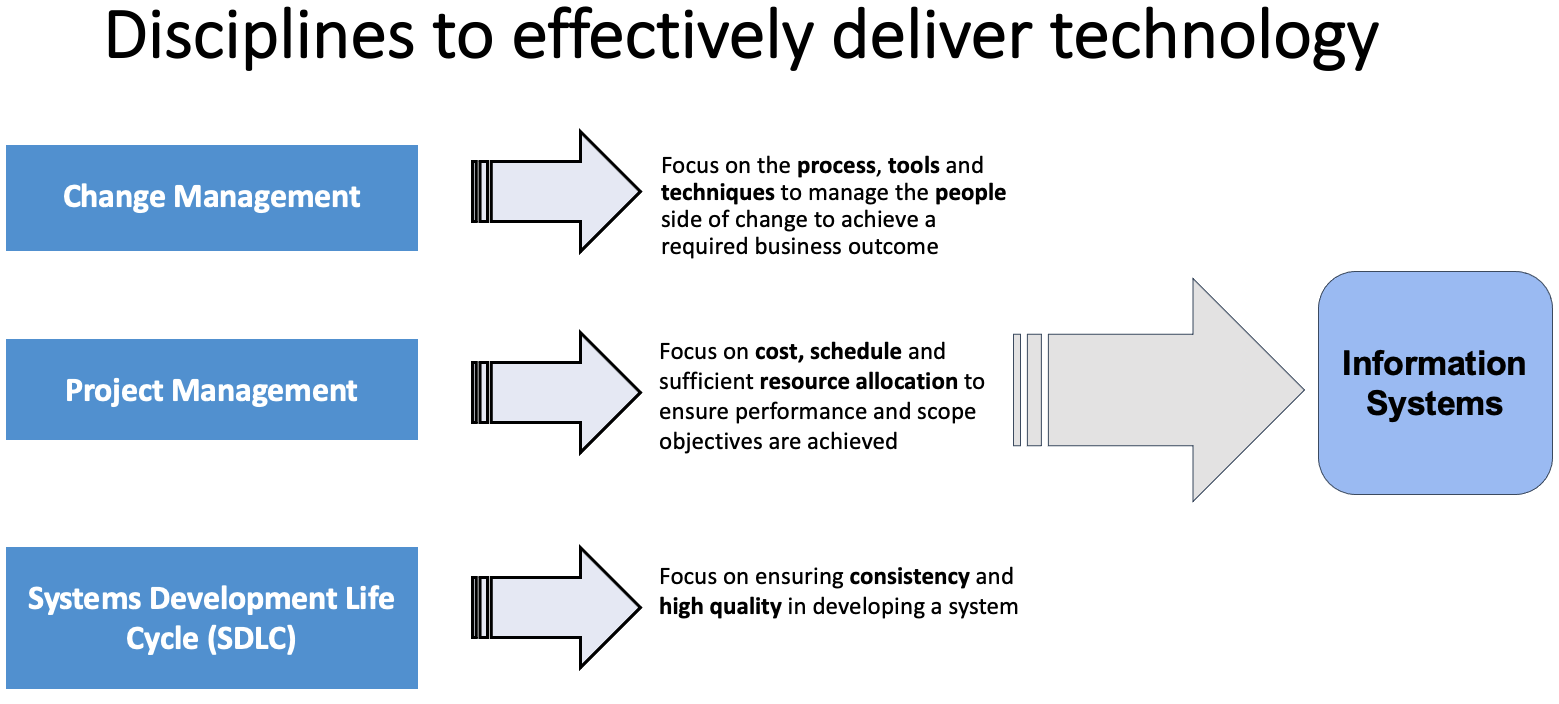
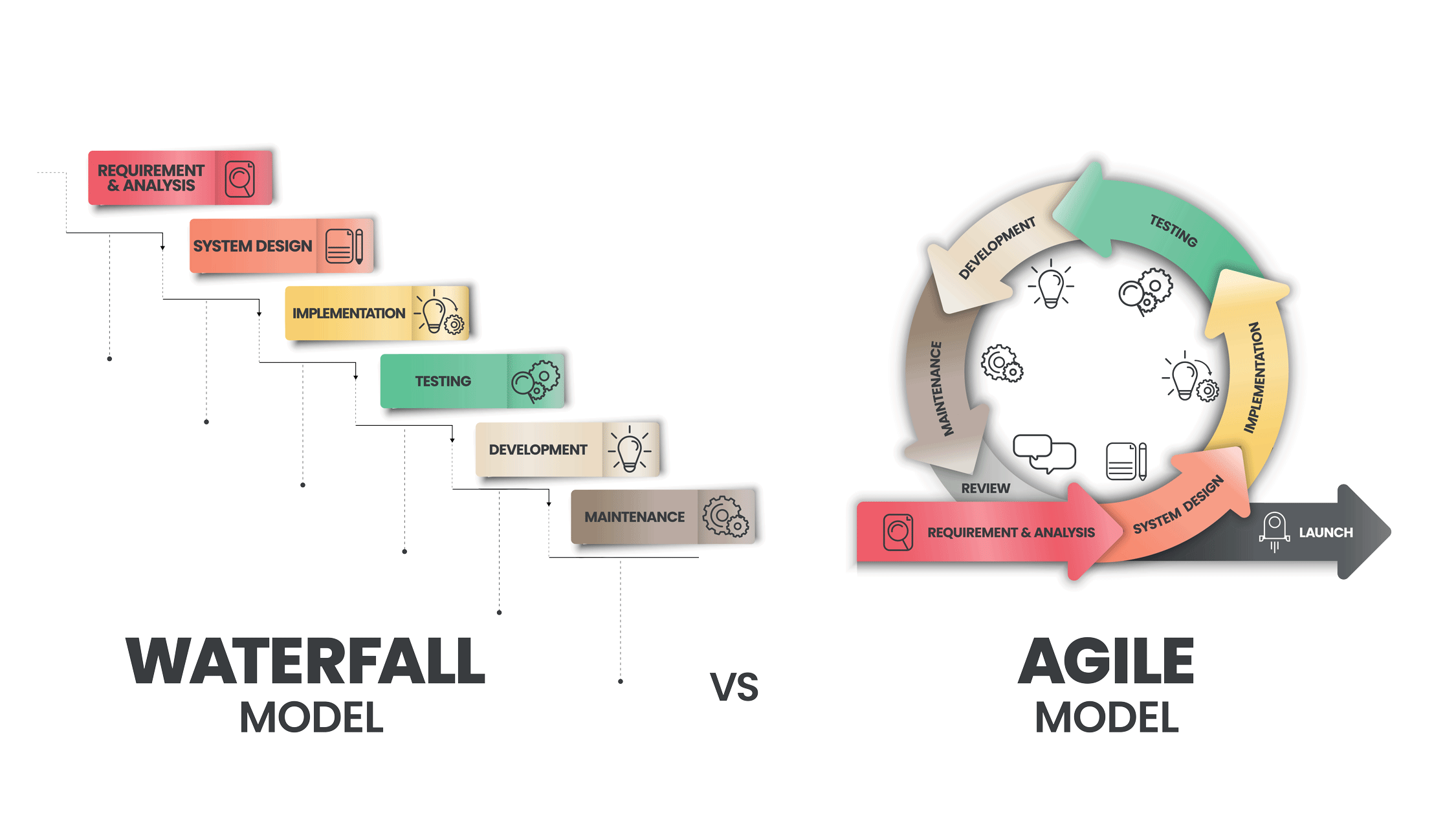
Based on the planning done through project management, and policies in effect within the jurisdiction, the development approach will focus on delivering a consistent and high-quality system either through a Waterfall, Agile or hybrid methodology.
While one is not necessarily better than the other, an Agile approach to systems development can be more flexible and dynamic in a rapidly changing world. Due to its continuous life cycle, the Agile approach can more readily apply additional functionality and choice in addressing user requirements. The Waterfall system development approach waits for the completion of user requirements before going into design, which can often cause the requirements to become outdated or unnecessary should there be a time lag between the two phases.
We are beginning to see a shifting system development paradigm that is being spearheaded by the Centers for Disease Control and Prevention (CDC) through its Data Modernization Initiative (DMI). Thinking about the challenges that lie ahead, CDC is considering lessons learned from the pandemic to strengthen the overall public health infrastructure with the Northstar Architecture roadmap and making fiscal, technical and workforce attributes key tenets of IIS sustainability.
The CDC plan will incorporate change management principles as part of the DMI initiative. Rather than merely focusing on the technology, clear, consistent and timely communication will provide guidance on policy and implementation, while partner engagement and autonomy will yield quicker decisions and better outcomes for communities.
We will also see more project management disciplines applied to DMI in the development of governance and standards for managing data collection and sharing across national partners, as well as consistent monitoring, tracking and reporting of progress toward targeted goals.
This is an opportune time for public health agencies to assess their own information systems and their organizations to become part of the data modernization effort. The assessment should be done through a concerted convergence of change management, project management and system development life cycle methodologies to bring both their partners and systems up to date.
This post was authored by Marcey Propp, and first published in the HLN Blog. It is reprinted by Open Health News with permission. The original post can be found here.
