How Antibiotic Pollution Of Waterways Creates Superbugs
 Humans pollute the world with many chemicals and some of these affect living things, even at very low concentrations. Endocrine-disrupting compounds, which interfere with hormones, are a good example, but recently more concern has been raised about pollution with antibiotics. The problem is that up to 80% of an antibiotic dose passes straight through the body. So most of the antibiotics used in medical treatment or during animal production may end up in waste water. And waste treatment plants generally don’t remove antibiotics very well.
Humans pollute the world with many chemicals and some of these affect living things, even at very low concentrations. Endocrine-disrupting compounds, which interfere with hormones, are a good example, but recently more concern has been raised about pollution with antibiotics. The problem is that up to 80% of an antibiotic dose passes straight through the body. So most of the antibiotics used in medical treatment or during animal production may end up in waste water. And waste treatment plants generally don’t remove antibiotics very well.
Antibiotic pollution also comes from spreading manure on crop land, or using sewage as fertilizer. Waste water released from hospitals and antibiotic production plants is another major source. We would like to know how much antibiotic pollution there is, but the diversity of antibiotic compounds makes it difficult to measure all of them at once. It’s also hard to estimate the amount of antibiotics used globally each year. But most researchers agree that total agricultural and medical use exceeds 250,000 tons per year.
How much pollution?
Using this number, we can make a very rough calculation about the extent of antibiotic pollution. If, say, 50% of an antibiotic dose is subsequently excreted, then 125,000 tons of antibiotics are released into the environment each year. This of course does not count release from pharmaceutical plants, which are very significant. Antibiotics are then likely to find their way into rivers, lakes and dams.
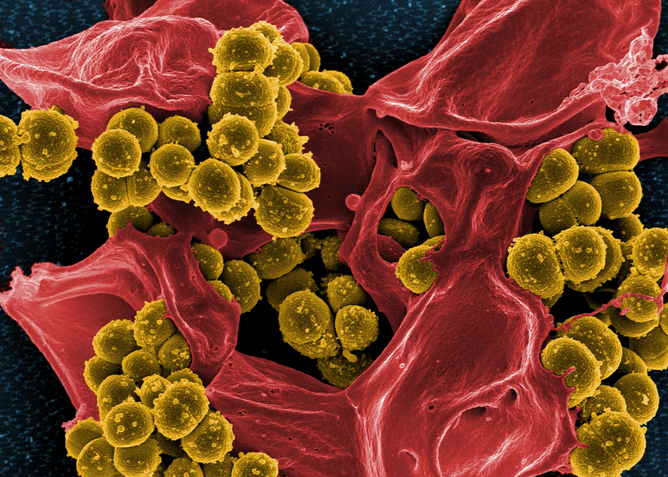 Antibiotic-resistant Golden Staph (Staphylococcus aureus) cells against a dead human white blood cell (false color image). NIAID/Flickr, CC BY-SAIn total, such freshwater sources contain 90,000 cubic kilometers of liquid water. This makes 12.5 x 1016 micrograms of antibiotic released into 9 x 1016 liters of freshwater each year. This results in a final concentration of about 1.4 micrograms per liter. This back-of-the-envelope calculation agrees surprisingly well with a growing number of reports on concentrations of particular antibiotics in waterways.
Antibiotic-resistant Golden Staph (Staphylococcus aureus) cells against a dead human white blood cell (false color image). NIAID/Flickr, CC BY-SAIn total, such freshwater sources contain 90,000 cubic kilometers of liquid water. This makes 12.5 x 1016 micrograms of antibiotic released into 9 x 1016 liters of freshwater each year. This results in a final concentration of about 1.4 micrograms per liter. This back-of-the-envelope calculation agrees surprisingly well with a growing number of reports on concentrations of particular antibiotics in waterways.
Of course, concentrations vary depending on how close you are to sources of antibiotic pollution. On the low end, Lake Baikal in Russia contains about one fifth of the world’s freshwater, but has little or no input of antibiotics.
At the other extreme, waste waters downstream from antibiotic production plants may contain antibiotics at levels hundreds of times higher than those found in the bloodstreams of people on antibiotic therapy.
Pollution and resistance
The consequences of this pollution are potentially very serious. Where the concentration of antibiotics is enough to inhibit bacterial growth, it’s almost certain to result in the appearance of antibiotic-resistant strains.
 Lake Baikal in Russia contains about one fifth of the world’s freshwater, but has little or no input of antibiotics. neverbutterfly/Flickr, CC BY
Lake Baikal in Russia contains about one fifth of the world’s freshwater, but has little or no input of antibiotics. neverbutterfly/Flickr, CC BY
This happens because microorganisms in the environment collectively carry and share enormous numbers of genes for resistance, virulence and other general nastiness. These genes can hop from one bacterial species to another, and the presence of antibiotics favors cells that have acquired these genes for resistance.
This allows existing pathogens to gain new forms of resistance, making them “super bugs” that are immune to all current antibiotics. Also, previously benign bacteria can acquire genes that transform them into emerging pathogens.
Even very low antibiotic concentrations have significant biological and evolutionary effects. Low, “sub-clinical” concentrations of antibiotics fall well below the concentrations used in antibiotic therapy. These concentrations do not kill bacteria. But they do induce bacteria to increase their rates of mutation, DNA recombination, and the rate at which genes hop from cell to cell.
Each of these changes at the DNA level can give advantages to bacteria, such as survival in the presence of heavy metals, disinfectants or antibiotics. So antibiotic pollution makes it vastly more likely that bacteria will become resistant or colonize new hosts, including humans.
Both the World Health Organization and the US Centers for Disease Control have identified antibiotic resistance as a high priority for research. We can help prevent resistance by using antibiotics wisely, by not dumping unused antibiotics in drains or toilets, and by improving water treatment.
We can also call for restrictions on the use of antibiotics as growth promoters in animal production, which actually accounts for the majority of antibiotic use worldwide. Australia has stringent regulations on the use of antibiotics in farm animals, but this cannot be said of elsewhere in the world. And in the modern age of rapid transport, a superbug in the United States, China or India will inevitably make its way to Australian shores.
Resistance is everyone’s problem.
![]()
Michael Gillings is Professor of Molecular Evolution
This article was originally published on The Conversation. Read the original article.
- Tags:
- antibiotic pollution
- antibiotic pollution of waterways
- antibiotic production plants
- bacterial mutation
- DNA recombination
- emerging pathogens
- endocrine-disrupting compounds
- hospitals waste water
- Michael Gillings
- pharmaceutical plants
- spreading manure on crop land
- superbugs
- US Centers for Disease Control (CDC)
- use of antibiotics as growth promoters in animal production
- using sewage as fertilizer
- waste treatment plants
- waste water
- World Health Organization (WHO)
- Login to post comments