US Senate Releases Draft Future Pandemic Preparedness Plan - Asks for Feedback
 Noam H. Arzt, Ph.D.The US Senate is asking for feedback on their pandemic preparedness plan. It is time for them to consider open source solutions that are being used successfully in the rest of the world.
Noam H. Arzt, Ph.D.The US Senate is asking for feedback on their pandemic preparedness plan. It is time for them to consider open source solutions that are being used successfully in the rest of the world.
On June 10, 2020 the US Senate released a white paper titled "Preparing for the Next Pandemic" under the signature of Senator Lamar Alexander of Tennessee. The white paper has five recommendations to address future pandemics based on lessons learned from COVID-19 and the past 20 years of pandemic planning. "The five recommendations...along with a series of questions at the end of this white paper, are intended to elicit recommendations that Congress can consider and act on this year," Senator Alexander said in a statement, adding that "I am inviting comments, responses, and any additional recommendations for the Senate Committee on Health, Education, Labor and Pensions to consider. This feedback will be shared with my colleagues, both Democrat and Republican." This feedback from the public will be accepted until June 26, 2020 and can be submitted to [email protected].
This nearly forty page document details a history of past Federal efforts since the mid 1990's to prepare for a pandemic in some detail, including specific legislative and funding initiatives. It then goes on to offer "lesson learned" and specific recommendations in five areas. The retrospective is actually rather interesting (I worked on a number of the projects identified in there over the years) and at least to my general recollection it seems accurate enough. I can't recall whether there is any major error of omission that might have painted an incorrect picture. The recommendations are generally sensible as well.
My particular interest is in public health informatics, so I focus on those areas of the white paper that are relevant to the funding and execution of systems and activities to support the informatics needs of managing a pandemic. Much of that falls in the area of disease reporting from clinical care to public health agencies, and the processing by the Centers for Disease Control and Prevention (CDC) of data it receives from state, local, tribal, and territorial public health agencies into summaries that drive national health policy.
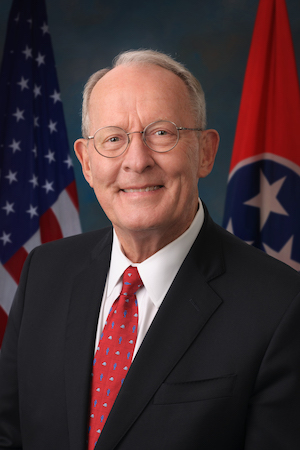 Senator Lamar AlexanderGiven the distributed nature of public health described elsewhere in this white paper, CDC has an added responsibility to provide as much coordination as possible for these activities. While funding of major public health organizations like the National Association of County Health Officials (NACCHO), the Association of State and Territorial Health Officials (ASTHO), Association of Public Health Laboratories (APHL), and the Council of State and Territorial Epidemiologists (CSTE) is a good start, coordinating bodies like the Joint Public Health Informatics Taskforce (JPHIT) have fallen by the wayside just when we needed them the most.
Senator Lamar AlexanderGiven the distributed nature of public health described elsewhere in this white paper, CDC has an added responsibility to provide as much coordination as possible for these activities. While funding of major public health organizations like the National Association of County Health Officials (NACCHO), the Association of State and Territorial Health Officials (ASTHO), Association of Public Health Laboratories (APHL), and the Council of State and Territorial Epidemiologists (CSTE) is a good start, coordinating bodies like the Joint Public Health Informatics Taskforce (JPHIT) have fallen by the wayside just when we needed them the most.
The report makes a strong recommendation for Congress to fund the Public Health Data Systems Modernization Act which is included in the Lower Health Care Costs Act introduced in the Senate in July 2019. This is additional funding to supplement the $50 million appropriated by Congress in FY2020 as part of its public health data systems modernization initiative, and an additional $500 million allocated as part of the CARES Act for "public health data surveillance and analytics infrastructure modernization" including a requirement that CDC report to Congress "on the development of a public health surveillance and data collection system for coronavirus within 30 days" of enactment of the Act. I don't really know where this money is going or how it is being used, but it is important to ensure sustained, long-term for public health information management at all levels of government.
The FY2021 Health and Human Services budget appropriate justification document has just two pages on public health preparedness and response, and the primary focus is on the Laboratory Response Network (LRN) which is an important but not solitary initiative. For pandemic response, recommendations to Congress should include more pointed direction to CDC to allocate funding to continue implementing electronic case reporting (eCR), and fund states to improve their disease surveillance systems as well as electronic laboratory reporting. The national eCR strategy is developed and has had initial implementation, and a new project called eCR Now is trying to prime the pump and increase participation.
Barriers to entry for electronic health record (EHR) participation in eCR are still a bit high due to the data they need to have available and especially their support of the required HL7 standards. Much of the focus these days is shifting to data interoperability using the Fast Health Interoperability Resources (FHIR) standard. For eCR, there is both a native FHIR specification which is not yet implemented, and a bridging strategy which uses an open source back-end SMART app which queries an EHR via older FHIR standards and generates an HL7 C-CDA electronic Initial Case Report (eICR) that most EHRs can't generate themselves.

For public health agencies, their systems have not had sufficient investment to be able to absorb eCR data routinely, so funding is needed to help public health agencies at all levels to improve their systems. It is also important to recognize the innovation that is part of the national eCR initiative. For example, one key component is the Reportable Conditions Knowledge Management System (RCKMS) which provides modern clinical decision support (CDS) services specific to every jurisdiction to help clinicians determine what conditions are reportable and how that reporting needs to be done.
Finally, one often-neglected fact is the severe lack of leverage of open source solutions to help with all this in the United States, which is not the case in much of the rest of the world. CDC does not seem to have a particular stance on this and that affects how the open source market reacts. And it is not really any better elsewhere in the Federal government (look at VA's replacement of VistA with Cerner's system as an example). The US is missing an opportunity to draw upon a wealth of available open source software well-established in healthcare (like openEHR and OpenMRS) successfully being used for COVID-19 response elsewhere in the world. To make matters worse, many of these projects are funded and developed by US-based contributors. Congress would get more "bang for its buck" with greater emphasis on using existing and new open source solutions.
- Tags:
- Association of Public Health Laboratories (APHL)
- Association of State and Territorial Health Officials (ASTHO)
- CARES Act
- Centers for Disease Control and Prevention (CDC)
- Cerner
- Clinical Decision Support (CDS)
- coronavirus
- Council of State and Territorial Epidemiologists (CSTE)
- COVID-19
- COVID-19 response
- data interoperability
- disease reporting from clinical care
- disease surveillance systems
- eCR Now
- electronic case reporting (eCR)
- Electronic Health Record (EHR)
- electronic Initial Case Report (eICR)
- Emergency Preparedness and Response (EPR)
- Fast Health Interoperability Resources (FHIR)
- FHIR specification
- future pandemics
- HL7 standards
- Joint Public Health Informatics Taskforce (JPHIT)
- Laboratory Response Network (LRN)
- Lamar Alexander
- Lower Health Care Costs Act
- National Association of County Health Officials (NACCHO)
- national health policy
- Noam H. Arzt
- open health
- open source back-end SMART app
- open source market
- open source software (OSS)
- open source solutions
- openEHR
- OpenMRS
- pandemic
- pandemic planning
- pandemic preparedness
- public health
- public health agencies
- public health analytics
- public health data collection
- public health data surveillance
- Public Health Data Systems Modernization Act
- public health data systems modernization initiative
- public health informatics
- public health information management
- public health infrastructure
- public health organizations
- public health surveillance
- Reportable Conditions Knowledge Management System (RCKMS)
- Senate HELP committee
- US Senate
- VistA EHR
- Login to post comments