Will PHIEs Lead the Consumer Medical Record Revolution and Bridge the Gap Between Personal Health Records and EHRs?
 Cora AlisuagIt has only been about two generations since traveling medicine shows were common forums for medical information. Phony research and medical claims were used to back up the sale of all kinds of dubious medicines. Potential patients had no real method to determine what was true or false, let alone know what their real medical issues were.
Cora AlisuagIt has only been about two generations since traveling medicine shows were common forums for medical information. Phony research and medical claims were used to back up the sale of all kinds of dubious medicines. Potential patients had no real method to determine what was true or false, let alone know what their real medical issues were.
Healthcare has come a long way since those times, but similar to the lack of knowing the compositions of past medical concoctions and what ailed them, today’s digital age patients still don’t know what is in their medical records. They need transparency, not secret hospital –vendor contracts and data blocking, like the practices being questioned by the New York Times. One patient, Regina Holliday resorts to using art to bring awareness to the lack of patient’s access to their own medical records.
There are many reasons patients want access. Second opinions, convenience, instant access in a medical emergency and right of ownership—I paid for them, I own them. Other reasons patients need to view their records is for accuracy and validity. Inaccurate record keeping has even caused the EHRI Institute to cite incorrect or missing data in EHRs and other health IT systems as the second highest safety concern in its annual survey, outlining the Top Ten Safety Concerns for Healthcare Organizations in 2015.
Healthcare system executives, from CIOs to CEOs are very aware of the increasing requirements from patients asking for their records and the various state and federal laws that come into play. However, they are also aware that by making it too easy for patients to access records they risk liability and HIPAA issues. They also don't want to provide documents that can easily enable cost comparisons or raise questions about charges.
Consumers Uniting
Riding the wave of interest in accessing personal medical records are organizations like GetMyHealthData.Org. The organization was founded in June 2015 as a collaborative effort among leading consumer organizations, health care experts, former policy makers and technology organizations that believe consumer access to digital health information is an essential cornerstone for better health and better care, coordinated by the National Partnership for Women & Families, a non-profit consumer organization. On July 4 it launched #DataIndependenceDay to create awareness for the HIPAA law which states that patients must be granted access to their health information with very few exceptions. An update to those laws that was finalized in 2013 extends these rights to electronic health records.
Despite the introduction of Personal Health Records (PHRs), Blue Button technology and product introductions from blue chip technology leaders such as Microsoft and Google, there has been no significant, unifying technology to ignite pent up demand for their medical records by consumers. This lack luster interest and ongoing interoperability issues might be the unifying force to drive many consumers to consider Personal Health Information Exchanges (PHIEs) as an alternative to EHRs and Health Information Exchanges (HIEs) that unnecessarily duplicate data and risk HIPAA violations.
Will PHIEs Ignite the Patient Record Access Movement?
Frost & Sullivan, in its research report, “Moving Beyond the Limitations of Fragmented Solutions Empowering Patients with Integrated, Mobile On-Demand Access to the Health Information Continuum,” identifies Personal Health Information Exchange (PHIEs). They are described as providing individual patients, physicians, and the full spectrum of ancillary providers with immediate, real-time access to medical records regardless of where they are stored by using an open API.
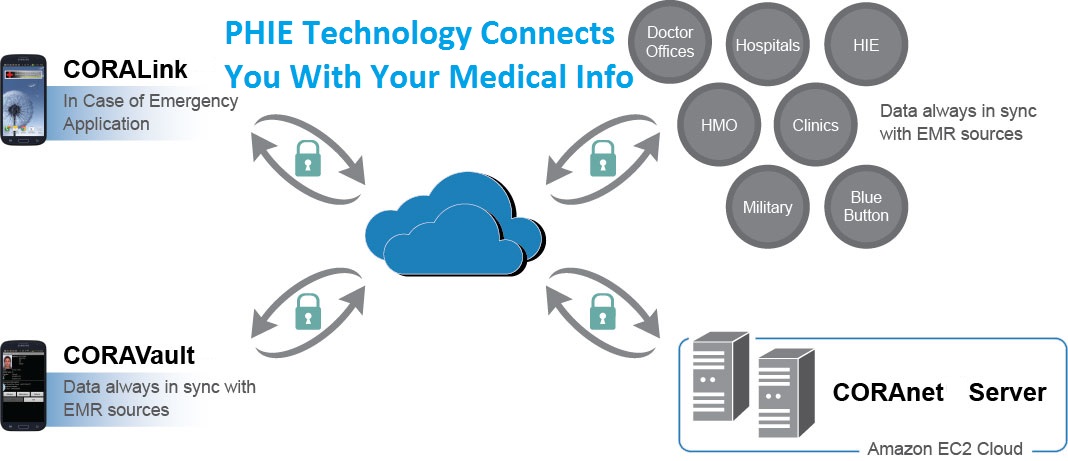 The PHIE can provide access to the entirety of an individual patient record, regardless of the number of sources or EHR systems in which the patient data resides. This technology is made possible through fully interoperable integration servers that can access any EHR system with available APIs and portray the integrated data in a viewable, secure and encrypted format on a mobile device.
The PHIE can provide access to the entirety of an individual patient record, regardless of the number of sources or EHR systems in which the patient data resides. This technology is made possible through fully interoperable integration servers that can access any EHR system with available APIs and portray the integrated data in a viewable, secure and encrypted format on a mobile device.
By leveraging the powerful simplicity of open APIs, PHIE technology can also access medical records in a way that is much more comprehensive than the closed EMR portals commonly used by doctors’ offices. Despite their pervasive use, these portals are cumbersome and expensive for patient’s use. The portals also include the same lack of interoperability that plagues hospital EHR systems.
“PHIEs can be the breakthrough everyone has been waiting for; challenging every consumer health organization, third-party payer, hospital, ACO network, and Congress to recognize the need to move away from proprietary systems. Adoption of this technology would also demonstrate the healthcare industries’ commitment to allowing patients access to their own records,” notes Dr. Donald Voltz, an anesthesiologist at Aultman Hospital in Canton, Ohio who leads a campaign for EHR connectivity.
“If done correctly, PHIEs can lead in the consumer health information campaign for change, interoperability now, quality and safety through license relationships with hospitals, payers, telecommunications companies, mobile device firms and large employers. Interoperability issues could be a thing of the past and lead to integration with leading EMR systems, integration with HIEs, VAR agreements with health and wellness IT firms and application distribution through the online market place with Google Play and iTunes," says Voltz.
Lack of Interoperability Continues to Hamper Patient Record Access
However, it has been six years since the HITECH Act passed, yet most Americans seeking medical care are still unable to obtain their full medical records for a variety of reasons. Some hospitals will simply not release them or proprietary EHR system vendors not allowing hospitals, let alone patients, direct access.
 This capability also comes at a critical time as enormous obstacles hamper the ability of people to obtain their medical records. This is documented in the ONC’s “2015 Report to Congress on Health Information Blocking” which concludes that it is apparent that some health care providers and health IT developers are knowingly interfering with the exchange of health information in ways that limit its availability and use to improve health and health care.
This capability also comes at a critical time as enormous obstacles hamper the ability of people to obtain their medical records. This is documented in the ONC’s “2015 Report to Congress on Health Information Blocking” which concludes that it is apparent that some health care providers and health IT developers are knowingly interfering with the exchange of health information in ways that limit its availability and use to improve health and health care.
This situation is only going to worsen as the Centers for Medicaid and Medicare (CMS) is considering a change to the EHR meaningful use rule that requires five percent of patients must view or download or transmit their health data to only one patient; not one percent, one patient.
Blue Button Not Gaining Traction
In the meantime, other PHR technology has been introduced but has not gained popularity including forays from Microsoft and Google. The ONC and other government organizations’ initiative to adopt and use the Blue Button platform for exchanging healthcare data between clinicians equipped with electronic health-record systems and patients with mobile computing devices is stalled, according to a recent survey by the not-for-profit Workgroup for Electronic Data Interchange (WEDI). WEDI questioned 274 providers, health plans, HIT vendors and claims clearinghouses in the Second Annual Survey of Industry Awareness of Blue Button, conducted late in 2014. Only eight percent of respondents noted that their organizations actually used Blue Button, down from 15% of survey respondents in 2013.
PHRs Largely Unpopular
PHRs joined the lexicon of medical terminology several years ago as a convenient way for consumers to have copies of their medical records. It was largely born out of EHR’s lack of interoperability and access. However, as far back as 2009, a Health Affairs article detailed the major factors behind the slow adoption of PHRs. The article reviewed some of the reasons and includes cost, access, interoperability, security concerns, and data ownership.
Because health records which include clinical data, laboratory results and medical images do not flow freely among multiple organizations due to lack of EHR interoperability, PHRs do not automatically receive data. This means that the data must often be entered manually by consumers—a time-consuming and error-prone process. For most consumers, this lack of safe and reliable automation makes it problematic to maintain a PHR, and a PHR that is not up-to-date likely will not be used. Unlike PHIEs, the API-EHR connectivity connection is the missing link in PHRs. However, the authors of the Health Affairs article offered a challenge. They described a gap between today’s personal health records (PHRs) and what patients say they want and need from this electronic tool for managing their health information. They noted that until that gap is bridged, it is unlikely that PHRs would be widely adopted, but noted that in the future; when these concerns are addressed, and health data is portable and understandable in content and format, PHRs will likely prove to be invaluable.
“While we all agree that lack of interoperability continues to stymie patient health record access and PHRs might not be the ultimate solution, but if a PHIE can bridge the gap by accessing EHR data through an open API while offering the security and convenience of a PHR. I believe PHIEs offer a solution that should satisfy the spontaneity of millennials' and more frequent use of middle-aged and elderly users,” says Tiffany Casper, RNC, CNM, MSN and President of EMR Consultants which helps medical organizations transition to EMR systems.
- Tags:
- Adam Dole
- Application Program Interface (API)
- Blue Button Connector
- Centers for Medicaid and Medicare (CMS)
- Cora Alisuag
- CORAnet Integration Server
- CORAnet Solutions
- CORAVault
- data integrity
- Donald Voltz
- Electronic Health Record (EHR)
- emergency situations
- Health Affairs
- Health IT Interoperability
- Healthcare 2.0
- HITECH Act
- In Case of Emergency (ICE) Solution
- lack of EHR interoperability
- Marc Wine
- Meaningful Use
- medical record access
- mobile device
- Mobile PHIE
- open API
- open source technology
- patient electronic medical record
- Paul Tibbits
- Personal Health Information Exchange (PHIE)
- personal health record (PHR)
- Login to post comments