We Are Going to Need Bigger Post-ITs if We Want Design Thinking in Healthcare
 Kim BellardI read a couple of stories on design thinking recently, which I'll get to shortly, but first I want to cite a well-known design maxim, usually attributed to designer Paul Rand:
Kim BellardI read a couple of stories on design thinking recently, which I'll get to shortly, but first I want to cite a well-known design maxim, usually attributed to designer Paul Rand:
If you can't make it good, make it BIG;
If you can't make it big, make it RED!
When it comes to healthcare, we certainly have a lot of things that are big, and probably the only reason more aren't red has to do with that color-of-blood/code red thing. But when it comes to design that one would really call good...not so much.
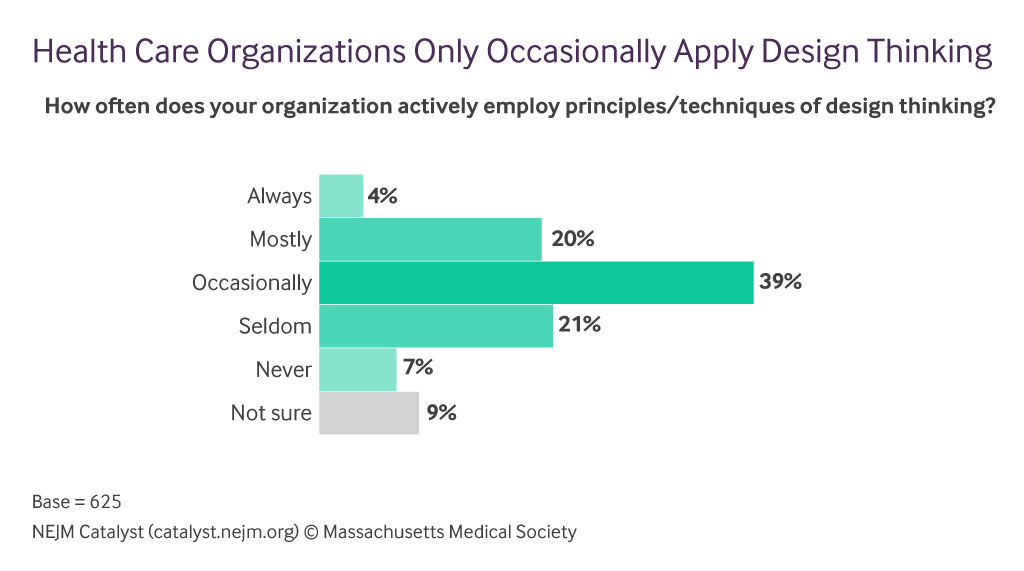
In NEJM Catalyst, Amy Compton-Phillips and Namita Seth Mohta reported on their Care Redesign Survey, which surveyed the NEJM Catalyst Insights Council. The survey found that there was strong support for design thinking (90%+), and was seen as valuable for a wide range of health care issues. Yet less than a quarter use design thinking regularly. When asked to list the top three barriers to applying design thinking to healthcare problems, respondents said:
- limited buy-in from decision-makers (52%),
- limited understanding of design (47%),
- insufficient design training (32%),
- uncertainty about ROI (28%),
- uncertainty about how it is different from other process improvement methods (27%),
- unclear ownership of design thinking (26%),
- identifying major problems may require overhaul of certain kinds of procedures (26%),
- patient needs don't always align with clinician needs (24%),
- No access or resources for technology/innovation experts (19%).
Clearly, a big part of the problem is not understanding design thinking or design, and how they should fit into everyone's job. Still, having about a quarter cite the possibility that procedures might have to change (oh, no!) suggests a certain inertia that is troubling, and that another quarter is worried that patients needs might be in conflict with clinician needs raises the question of for whom the system exists.
As Stacey Chang, Executive Director at the Design Institute for Health at the University of Texas at Austin, put it: “The dysfunction of our modern health care system isn’t about failure of intention, but rather pursuit of siloed and sometimes conflicting priorities.”
I'm shocked, shocked...
The authors conclude, hopefully:
In this new era of patient-driven care delivery, it’s not enough to adapt existing systems; we need to create something better. Design thinking can get us there.
Designer Jon Kolko might not be so sanguine. In a recent article, he notes a backlash against design thinking -- it is "kind of like syphilis;" it is "bullshit;" it is a "failed experiment" -- and worries that it "has warped into something superficial."
It isn't that Mr. Kolko is against design thinking; not at all. He just thinks that too much of it isn't being done by "people and firms practicing design thinking by making things, driven by practitioners aware of the history of making things and skilled in the craft of making things."
As he laments:
It’s safe to say that most people practicing popularized design thinking haven’t explored the psychology of problem solving, the history of union-led interventions in Scandinavia, or the idea of design as a liberal art...Similarly, they probably haven’t spent years drawing, building and modeling, and giving detailed form to complex ideas.
He summaries the critiques of design thinking as follows:
- "It takes a thoughtful, complex, iterative, and often messy process and dramatically oversimplifies it in order to make it easily understandable.
- It trivializes the role of craft and making things, which is fundamental to the process of design.
- It promotes “empathy lite”—as if an empathetic and meaningful connection with people could be forged in hours or even days.
- It’s become a tool of consultancies to sell work, not to drive real impact."
 Credit - Giorgio Montersino CC BY SA 2.0Put more succinctly, "today’s design thinkers lack craft, lack intellectual foundations, and can’t make things." Ouch.
Credit - Giorgio Montersino CC BY SA 2.0Put more succinctly, "today’s design thinkers lack craft, lack intellectual foundations, and can’t make things." Ouch.
Instead, he says, we have workshops, TED talks, subject-matter experts, working sessions, and the like. The result: "And instead of beautiful, usable, significant, and relevant designed things, we have “canvases” and “playbacks” and “design sprints”—and lots and lots of Post-it notes."
You knew the Post-it notes had to fit in here somewhere.
As critical as Mr. Kolko is about how much of design thinking is being done now, he sees a silver lining:
Organizations seek silver bullets, and they’ve moved from the shiny objects of Six Sigma to agile to lean to design thinking. It is guaranteed that companies will move on from design thinking to the next big thing. But in its wake, the popularity of design thinking will leave behind two benefits: validation of the design profession as real, intellectual, and valuable—and a very large need for designers who can make things.
In other words, leave it to the professionals.
I'm somewhere in the middle. Too many of healthcare's problems are because we've left them to the professionals. Too often those professionals end up thinking more about their own interests (patients needs not aligned with clinicians' needs???) or don't really understand how people actually use things in the healthcare system (case in point: EHRs).
It doesn't have to be this way. For example, a research team at University of Pennsylvania wrote in Fast Company about how they've "reimagined" EHRs by designing them alongside clinicians. They call for "the kind of co-creation among clinicians and developers we expect from contemporary design in other industries."
Now if only design could also involve patients and everyone else involved in the system.
Design thinking is not a magical bullet. But it is something we should all be mindful of, all the time. How do we improve things? How do we make things easier? How will this impact that, and them? Similarly, design isn't a magic bullet either. We have some lovely healthcare buildings that look pretty but that still manage to be confusing and scary places for patients and their loved ones.
It's easy to take a too narrow view of what design includes and whom it impacts. Apple's products look great and have slick packaging, sure, but their success comes more because they are easy to use and do what users want, in ways they understand.
Until we get to that point, bring on the Post-its.
| We're Gonna Need Bigger Post-Its if We Want Design Thinking in Healthcare was authored by Kim Bellard and first published in his blog, From a Different Perspective.... It is reprinted by Open Health News with permission from the author. The original post can be found here. |
- Tags:
- Amy Compton-Phillips
- Care Redesign Survey
- Design Institute for Health
- design thinking
- dysfunction of modern health care system
- health care issues
- healthcare
- human factor engineering (HFE)
- Jon Kolko
- Kim Bellard
- Namita Seth Mohta
- NEJM Catalyst
- NEJM Catalyst Insights Council
- patient-driven care delivery
- Paul Rand
- Post-it notes
- Stacey Chang
- University of Pennsylvania
- University of Texas at Austin
- usability (UX)
- Login to post comments